251
Views & Citations10
Likes & Shares
HIV testing among men remains low globally and in sub-Saharan Africa in particular, when compared with their female counterparts. The study is aimed at synthesizing evidence on barriers to HIV testing among men in Ogoja Cross River State Nigeria using a scoping review method. A scoping review were conducted, guided by Arksey and O'Malley's framework.
STATEMENT OF THE PROBLEM
HIV testing among men remains low globally and in sub-Saharan Africa in particular, when compared with their female counterparts. Less than a quarter of the adolescent and young adult (23.7%) had ever tested for HIV, and an even lower proportion (12.4%) tested in the year preceding the survey. More females (25.4%) compared to males (20.8%) had ever tested for HIV. The study was aimed at investigating into the root cause(s) of low HIV testing uptake among men in Ogoja, Cross River Sate and recommend possible solution to the identified barriers in order to improve HIV testing coverage among men in Ogoja.
RESEARCH QUESTIONS OF THE STUDY
The study answered the question below:
- What factors prevent men from receiving HIV testing services in Ogoja?
RESEARCH HYPOTHESIS OF THE STUDY
- There is negative relationship between fear of HIV positive result and HIV testing among men.
- There is positive relationship between knowledge of HIV and HIV testing uptake.
- There is negative relationship between stigma and HIV testing uptake.
- There is positive relationship between confidentiality and HIV testing uptake among men.
- There is positive relationship between good attitude of health care service providers and HIV testing uptake among men.
OBJECTIVES OF THE STUDY
General Objective
To study the key barriers to HIV testing uptake among men in Ogoja Cross River Sate Nigeria.
Specific Objectives
- To explore barriers to HIV testing among men in Ogoja.
- To examine possible recommendations to improved HIV testing among men in Ogoja.
Significance of the study
The primary beneficiaries of the findings of this study are the public health sector as this helps public health workers develop strategies to improved HIV testing among men, which will help to break the chain of HIV transmission. It also provides a systematic body of knowledge that can be explored for appropriate policy formulation, act as a reminder to both the state and civil society to always incorporate policy that improved HIV testing uptake among men. findings also provide guidance to health care facilities in Ogoja area in planning for strategies to improve HIV testing services rendered to men.
LITERATURE REVIEW
Comprehensive testing for HIV infection is critical to addressing the HIV pandemic globally. Effective testing improves surveillance, aiding in evaluating prevention efforts, and ensures that HIV-infected individuals can be engaged in care early, avoiding preventable morbidity and mortality [1]. Regrettably, access to testing is often inadequate in Low- and middle-income countries where the burden of HIV is greatest.
CONCEPTUAL FRAMEWORK
HIV
HIV (human Immunodeficiency virus) is also an epidemic that attacks cells that facilitate the body fight infection, making somebody extra in danger of different infections and diseases. It's unfolded by contact with sure bodily fluids of somebody with HIV, most typically throughout unprotected sex (sex whereas not a security or HIV medication to forestall or treat HIV), or through sharing injection drug instrumentation.
If left untreated, HIV can cause the illness AIDS (acquired disorder syndrome).
The physical structure can’t get eliminate HIV and no effective HIV cure exists. So, once you have HIV, you have it forever.
However, by taking HIV medication (called antiretroviral treatment or ART), people with HIV can live long and healthy lives and forestall transmission HIV to their sexual partners. to boot, there are effective methods to forestall getting HIV through sex or drug use, at the side of pre-exposure prophylaxis (PrEP) and post-exposure Prophylaxis (PEP) [2].
First famed in 1981, HIV is that the rationale for one in each of humanity’s deadliest and most persistent epidemics.
HIV Test
ELISA (enzyme-linked immunosorbent assay): a screening looks at want to find infection with HIV. If positive, the enzyme-linked-immunosorbent serologic assay look at is sometimes recurrent.
Western blot: a look at typically want to make sure the results of associate enzyme-linked-immunosorbent serologic assay. It will rule out a false-positive by distinctive HIV antibodies from alternative antibodies which will react to the enzyme-linked-immunosorbent serologic assay.
IFA (indirect fluorescent associate antibody): a look at used just like the less costly Western blot to substantiate the results of an enzyme-linked-immunosorbent serologic assay.
The premiere looks at which will identify the genetic material, the RNA, of the HIV virus is named PCR (the enzyme chain reaction). PCR will find associate early HIV infection before associate antibodies area unit evident and verify whether a baby born to an HIV-positive mother can have HIV. A take a look at like PCR testing, known as the branched deoxyribonucleic acid, take a look at, additionally detects the ribonucleic acid of HIV.
Barriers
A barrier are some things sort of a rule, law, or policy that makes it difficult or inconceivable for one factor to happen or be achieved. Duties and taxes are the foremost obvious barrier to trade.
A barrier is also a drawback that stops a pair of us or groups from agreeing, act, or operational with each other [2].
The WHO estimates that in 2012 only half of all HIV-infected individuals in sub-Saharan Africa knew their serostatus. Fortunately, recently developed low-cost, rapid test formats capable of detecting HIV-related antibodies have helped improve access by removing the need for sophisticated laboratories and allowing same-day provision of test results. Awareness of HIV serostatus is especially important in the high-prevalence settings of most LMIC because it offers the opportunity to access treatment-often free or low-cost through subsidization in many resource-limited settings-and to make informed, responsible decisions about childbearing and avoiding transmission to partners. Given increasing anti-retroviral treatment (ART) availability, in 2006, the United Nations called for HIV testing services in resource-poor settings to be scaled up. Knowledge of HIV sero-status is a gateway towards ensuring universal access to HIV/AIDS prevention, treatment, and care. Furthermore, studies have demonstrated the efficacy of HIV testing in decreasing sexual risk behaviors in generally healthy populations. However, the literature has consistently reported a major gender gap in participation in HIV testing across Sub-Saharan African (SSA) countries, despite increased service availability. Recent national population surveys conducted in low- and middle-income countries, including Sub-Saharn Africa, showed that 12% of women and 7% of men report having had an HIV test in the previous twelve months, while 34% of women and 17% of men report ever having undergone HIV testing. The gender gap in testing has important implications since HIV testing gives the opportunity to engage in care programs and in secondary prevention, particularly so in countries where HIV prevalence is low. Men's utilization of HIV testing is essential because as household head, men control decisions and resources that are essential for HIV prevention and care among women. Still, the recent HIV literature on men has focused primarily on ART and their role in the Prevention of Mother to Child Transmission (PMTCT) services but has paid very limited attention to the analysis of male HIV testing patterns. Only a handful of studies, all of which applying exclusively either quantitative or qualitative methods has investigated individual and system structures likely to explain what compels men to undergo an HIV test. A study relying on a discrete choice experiment exploring stated preferences for testing among men and women pointed to the importance of heterogeneous gender-specific preferences in testing. In Burkina Faso, the few quantitative surveys on HIV testing status among men are limited either to the health facility visitors or to the professionals such as health workers or teachers.
In general, the literature has highlighted a positive association between the likelihood of men having tested for HIV and older age, better HIV knowledge, higher income, higher educational and socio-economic status. Proper understanding of the complexity of the decision-making process which leads men to undergo an HIV test is still missing.
Our mixed methods, population-based study relied on a combination of quantitative and qualitative methods to explore the complexity of the issue, by both measuring (quantitative) and explaining (qualitative) factors associated with men’s HIV testing behavior in Ogoja.
Barriers to HIV testing uptake among
Knowledge of HIV. Eleven of the studies included in this review reported evidence on knowledge of HIV among men in SSA [3-6], suggesting a generally high level of HIV knowledge among men in SSA [5].
Fear of testing positive for HIV Nine of the included studies reported evidence on fear of testing positive for HIV as a barrier to men’s uptake of HIV testing services in SSA [3,4,6,7]. Some of these studies indicated that men feared taking the HIV test due to the possibility of getting an HIV-positive result [4,6,7]. Others believed that the test did not give accurate results, while some feared for their personal relationships, that their wives or partners might leave or deny them sex once their HIV-positive status was known [3,6]. This extended to men not wanting to test for HIV with their wives or partners; in Zimbabwe, for example, only 7% had tested with their wives in Zimbabwe. Men do not want their partners to know their status so they do not test for HIV [7], fearing that they would be judged for infidelity or cheating should they test positive [6,7], or lose respect or dignity in their communities.
Stigma associated with HIV Fourteen articles reported evidence on stigma and HIV testing uptake among men [3-6,8]. Studies conducted in Malawi, Kenya and Uganda, two from South Africa, and one each from Ethiopia, North Africa and SSA found that the stigma associated with testing HIV-positive persists in many communities and negatively affects men’s engagement with HIV testing services [6,8] especially given reported incidences of health care facilities’ failure to protect confidentiality [5]. These findings were supported by other studies conducted in Uganda and Burkina Faso, which concluded that if men tested seropositive, their families as well as communities would easily tell that they were HIV-positive [5] which would unintentionally expose them to rejection [3], gossip and shame, and even lead to men committing suicide. As such, men were even scared to attend local clinics because they were worried that they might meet people from their neighborhoods. Health care providers and confidentiality Evidence on confidentiality and the level of trust towards health care workers was reported in 10 articles [4]. These articles revealed that men do not trust that their HIV-positive test results will, always, be kept confidential by the nurses at the clinics. Other studies indicated that men’s expectation of professionalism from health care workers was often undermined by health workers’ unsupportive and unfriendly reactions towards them [4]. This included poor quality of care [4], breaches of trust and concerns that health care workers would gossip about HIV test outcomes to community members. Some men displayed serious mistrust, even suspecting that health care workers were bribed by individuals to give incorrect HIV results. Men also refrained from HIV testing in local clinics, citing concerns that testing was conducted by counsellors from local communities, which threatened confidentiality [4]. Therefore, more people preferred self-testing as a possible alternative. Long queues and waiting periods of four to five hours at public clinics have also been cited as barriers to men’s health-seeking behavior and retention to ARV treatment [4].
Setting or location for HIV testing Evidence on the testing setting was discussed in 13 articles [3,4,6,7]. Studies conducted in South Africa, Ghana and SSA revealed that men generally felt that a public clinic setting make them feel uncomfortable to either test for HIV or collect ARV treatment [4] especially where there are local people known to them [6]. One of the reasons cited was that public clinic waiting rooms were full of female patients and female health care workers [4], and those men therefore avoided such “women-centered” facilities. Hence, many of them do not support their pregnant partners during antenatal visits. Further studies revealed that unsuitable operating hours in public clinics served as a barrier to many men accessing HIV testing services because they were at work during these times [7] and cited the importance of extended service hours at weekends and having testing services and ARV collection sites closer to where they worked or lived. This may be particularly beneficial to men who avoided services at clinics that are located within their communities. Masculinity Evidence on masculinity and HIV testing uptake was reported in eight articles. Studies conducted in Zimbabwe, Kenya and Uganda found that health-seeking behavior among men was an issue about masculinity which justified their reluctance to test for HIV, or admit to ill-health. A high number of men who died in 2011 did so because of poor health-seeking behavior, with 33% of men being lost to treatment between testing positive and initiating ART. Studies conducted in South Africa and Zimbabwe revealed that some men believed that an HIV-positive test result meant that they had to adopt a new lifestyle and that this diminished their masculinity and negatively impacted their manhood. This was supported by other studies from Uganda and Kenya which established that men were reluctant to test for HIV because they feared being considered “weak”, or losing dignity and respect if they tested HIV-positive. Even attending clinic with a spouse for HIV testing was uncommon and considered strange by some men, or ridiculed by other men. Sexual behavior and HIV. The extent to which men’s sexual behavior affected HIV testing uptake was reported in seven articles.
Conclusively, structural, and individual factors present barriers to HIV testing uptake among men in Sub Sahara Africa. Community and home-based initiatives have the potential to improve the uptake of HIV testing among men in Sub- Saharan Africa, considering the confidentiality concerns posed by clinic settings [9].
This study was conducted through an online survey system known as Mwater. A random sample of Ogoja Local Government Area’s men were selected and sent questionnaire with the link to the online survey. The survey includes a yes or No scale that, was used with perception questions. It also includes nominal questions (e.g., age, gender, race, and region. Stigma, HIV knowledge and confidentiality (independent variable) and HIV test uptake (dependent variable) was tested and analyzed, using percentages and frequencies.
The Study Area and Population
The study comprised of men between the ages of 18-64 years within Ogoja Local Government Area of Cross River State Nigeria. Ogoja is a Local Government Area in Cross River State, Nigeria. Its headquarters is Ogoja town in the northeast of the area near the A4 highway at6°39′17″N 8°47′51″E. It has an area of 972 km² and a population of 171,901 at the 2006 census.
Inclusion criteria
Men aged 18-64 years who resides in Ogoja and willing to participate in the study.
Exclusion criteria
Eligible subjects who decline to provide consent, men who are sick and unable to give information at the time of study and mentally challenged eligible subjects.
SAMPLING TECHNIQUES AND SAMPLE SIZE
Sampling Techniques
Sampling is the process or technique of selecting a suitable sample or a representative part of a population, for the purpose of determining parameters or characteristics of the whole population. List of all eligible men from each location in the study area were made with assistance from local leaders and community health volunteers; this was done prior to commencement of data collection. Simple random sampling was used to select 200 by using (N-n/N-(+N*e2 1) formulae. Here P is a probability, n is the sample size, and N represents the population. Now if one cancels (N-n/N-(+N*e2 1) it will provide P = n/N. Moreover, the chance of a sample getting selected more than once is needed: P = 1-(1-(1/N)). Each of the 10 wards within Ogoja Local government were represented in the sample population. This was continued until the desired sample size were achieved. Thus, the sample size was sufficient as the entire ward were represented, afterward generalization was made. Data Collection Instruments.
Semi-structured questionnaires were administered to all men. The questionnaires were administered by the online app (Mwater) with the help of research assistant who were trained by the researcher beforehand.
Data Analysis
After all data were collected, it was cleaned and coded for analysis. Data cleaning involved identification of incomplete or inaccurate responses then cross checking against original documents and corrected. After data cleaning, the data were coded and entered in the computer for analysis using the Statistical Package for Social Sciences (SPSS) 20.0. This study yielded both qualitative and quantitative data.
The frequency was used to assess differentials existing between various barriers of men to uptake of HIV test. Cross tabulation was used to display the nature of association between the study variables. P- Value of less than 0.05 were considered statistically significant. The results of data analysis were then presented using frequency distribution tables. The information was presented using proportions and percentages in tables, figures.
Data Presentation and Analysis
In this chapter, the data collected from the respondents are presented and analyzed here, for the sake of clarity; frequency counts and percentage were used (Table 1).
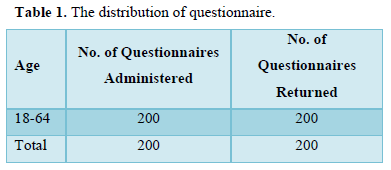
The table above indicates that out of 200 questionnaires earlier administered 200 were returned. The respondents administered to them are all male between the ages of 18 to 64 years.
- Are you afraid of testing for HIV because of been tested positive (HIV Virus in the blood) for HIV? (Table 2).
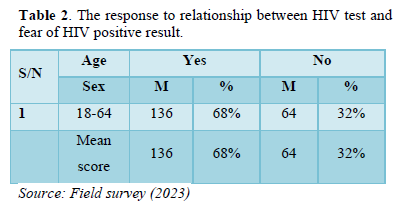
The result as shown in the table two above indicates that 136 male respondents of the sampled population representing 68 percent agreed that they are afraid of testing for HIV because of been tested positive for HIV and 64 male respondents of the sampled population representing 32 percent do not agreed that they are afraid of testing for HIV because of been tested positive for HIV.
- Did you not test for HIV because of lack of knowledge of HIV? (Table 3).
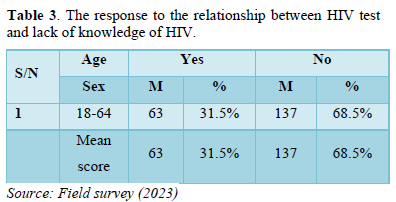
The result as shown in the table three above indicates that 63 male respondents of the sampled population representing 31.5 percent agreed that they didn’t test for HIV because of lack of knowledge of HIV and 137male respondents of the sampled population representing 68.5 percent do not agreed that they didn’t test for HIV because of lack of knowledge of HIV.
- Did you not test for HIV because of fear of stigma? (Table 4).
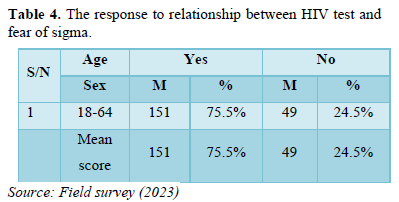
The result as shown in the table four above indicates that 151 male respondents of the sampled population representing 75.5 percent agreed that they didn’t test for HIV because of fear of stigma and 49 male respondents of the sampled population representing 24.5 percent do not agreed that they didn’t test for HIV because of fear of stigma.
- Did you not take HIV test because of lack of confidentiality in the service providers/Health care workers? (Table 5).
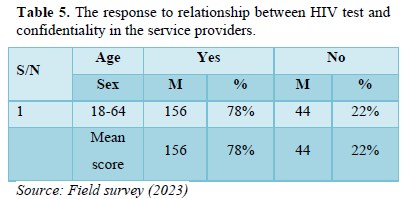
The result as shown in the table six above indicates that 156 male respondents of the sampled population representing 78 percent agreed that they didn’t test for HIV because of lack of confidentiality in the service providers or health care workers and 44 male respondents of the sampled population representing 22 percent do not agreed that they didn’t test for HIV because of lack of confidentiality in the service providers/health care workers.
- Did you hate taking HIV test because of attitude of the health care providers? (Table 6).
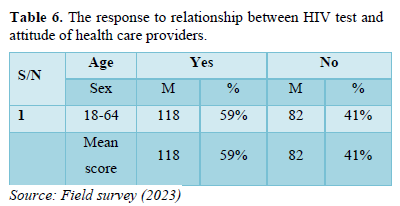
The result as shown in the table seven above indicates that 118 male respondents of the sampled population representing 59 percent agreed that they didn’t test for HIV because of attitude of health care providers and 82 male respondents of the sampled population representing 41 percent do not agreed that they didn’t test for HIV because of attitude of health care providers.
DISCUSSION OF RESULTS
The research conducted to discover possible barriers to uptake of HIV test among men in Ogoja Local Government of Cross River State, Nigeria and to see possible ways to increase HIV test coverage among the target population.
RESULTS
- It was discovered that 68% of men out of the sampled population were afraid of testing for HIV because of been tested positive for HIV. However, 32% of the population do not agree to that.
- It was ascertained that 63 male respondents of the sampled population representing 31.5 percent agreed that they didn’t test for HIV because of lack of knowledge of HIV and 137male respondents of the sampled population representing 68.5 percent do not agreed that they didn’t test for HIV because of lack of knowledge of HIV. Thus, knowledge of HIV is not a major barrier to uptake of HIV test among men.
- It was agreed that men didn’t test for HIV because of fear of stigma that is associated to HIV test as 75.5% of the population stated that fear of stigma prevent them from HIV test uptake.
- The result shows that 75 male respondents of the sampled population representing 37.5 percent agreed that they didn’t test for HIV in the facility because the setting is more of women whereas 125 male respondents of the sampled population representing 62.5 percent do not agreed that they didn’t test for HIV in the facility because the setting is more of women. It was deduced facility does not have significant effect on HIV testing among men.
- The result indicates that 156 male respondents of the sampled population representing 78 percent agreed that they didn’t test for HIV because of lack of confidentiality in the service providers or health care workers and 44 male respondents of the sampled population representing 22 percent do not agreed that they didn’t test for HIV because of lack of confidentiality in the service providers/health care workers. Following the result, trust in the service providers is a key barrier to HIV test uptake among men.
RECOMMENDATIONS
- Further exploration on barriers to uptake of HIV test among men is required.
- HIV counseling can be expanded to incorporate discussions around the non-health factors that men weigh in their decisions to get tested and they should be reassured of living well even if tested positive.
- Engagement of community stakeholders through community dialogue meeting to destigmatize HIV test and attitudinal change of the health care workers through effective communication skill and client centric service delivery for optimal confident in health care workers.
DISCUSSION
This study found that fear of positive test result, stigma, and lack of confident or trust in the service providers influences uptake of HIV test. The majority of the participants have fair knowledge of HIV virus. In addition to that, the majority of the participants also reported that facility setting that is more of women does not influence HIV test among men. Nevertheless, according to Hlongwa [9] key barriers to HIV testing among men in sub-Saharan Africa were knowledge of HIV, fear of testing positive for HIV, stigma associated with HIV, healthcare providers’ services, confidentiality, and clinic setting.
According to Mohlabane [10], fear of finding out one's HIV test result was reported by most (73%) participants as the biggest barrier to HIV testing, however, only 16% of those who had never been tested for HIV reported this to be a major barrier. Fearing what people may say was cited as the second biggest barrier (49%; 15% for non-testers) to HIV testing, followed by shyness or embarrassment (28%; 20% for non-testers) and avoidance of divulging personal information to health workers (24%; 19% for non-testers). Staff attitudes (3%; 19% for non-testers), lack of knowledge of testing sites (3%; 35% for non-testers) and lack of treatment availability (6%; 56% for non-testers) for HIV positive persons were reported among the least barriers to HIV testing. Only 2% of the participants reported inconvenient site opening hours as a barrier to HIV testing and none (0%) of those who had never been tested for HIV reported this to be the case.
The “other” category prompted respondents to mention any other barriers that were not mentioned under the list of barriers to HIV testing provided. Previous HIV testers specified the following factors as barriers to HIV testing: Fear of death (33%); Being uncertain of lifestyles which includes having too many partners and lack of condom use (20%); Being afraid of the stigma associated with HIV/AIDS and taking treatment for HIV (11%); Do not think that they are at risk (9%); In denial of HIV/AIDS (7%); Lack of understanding of the virus (6%); Being scared of what partners may say when one tests HIV positive (4%); Not being ready to test for HIV (4%); Travel costs to HCT sites (2%); Testing time (2%) and Lack of motivation to test (2%). For those who had never tested for HIV the “other” barriers were: Fear of death (33%); Being uncertain of lifestyles (28%); Not being ready to test (11%); Being afraid of stigma (11%); Lack of understanding of HIV (11%) and Lack of motivation to test for HIV (6%).
CONCLUSION
Structural and individual factors present barriers to HIV testing uptake among men in Ogoja. Community, home-based and HIV self-testing initiatives have the potential to improve the uptake of HIV testing among men in Ogoja, considering the confidentiality concerns posed by clinic settings.
A significant negative relationship between knowledge of HIV/AIDS contraction and facility setting more of women. This outcome signifies that as the level of stigma increases, the level of knowledge for HIV/AIDS contraction modalities increases.
LIMITATIONS
For this study include a small sample size and a narrow data collection time frame. Additional data collection time would have allowed for larger sample size and greater participant representation. The small sample size compromised the generalizability of the findings of this study. Implications for Future Research, Social Work Practice, and Policy From the results of this study, we suggest that social staff work towards educating the world and have interaction stakeholders through community dialogue meeting to destigmatize HIV look at, and other people living with HIV. we tend to suggest that policies are required to advocate for individuals living with HIV. Social staff ought to advocate for PLWHA to cut back health disparities and participate within the hindrance of HIV/AIDS. The results of this analysis will be used towards support exaggerated HIV education for world.
CONCLUSION
This study was conducted to research barriers to HIV test among men, vital findings of the study conclude: fear of positive test result, stigma and trust impact uptake of HIV test.
Researchers recommend additional analysis and examination of underrepresentation sampled population. Researchers additionally recommend that social staff ought to destigmatize HIV test, strengthen angle of health care staff to produce client central services and policy formulation that deterred potential perpetrators of sigma.
- Reynolds SJ, Thomas C (2017) Quinn, in Infectious Diseases. Available online at: https://study.com/academy/lesson/what-is-sampling-in-research-definition-methods-importance.html
- Agada SJ, Ezekiel P (2023) Barriers to HIV Testing among Clients of Female Sex Workers an Assessment of Ogoja Local Government Area. Texila Int J Public Health 11: 1-10.
- Obermeyer CM, Sankara A, Bastien V, Parsons M (2009) Gender and HIV testing in Burkina Faso: An exploratory study. Soc Sci Med 69(6): 877-884.
- Leichliter JS, Paz-Bailey G, Friedman AL, Habel MA, Vezi A, et al. (2011). Clinics aren’t meant for men: Sexual health care access and seeking behaviors among men in Gauteng province, South Africa. SAHARA J 8(2): 82-88.
- De Allegri M, Agier I, Tiendrebeogo J, Louis VR, Yé M, et al. (2015) Factors Affecting the Uptake of HIV Testing among Men: A Mixed-Methods Study in Rural Burkina Faso. PLoS One 10(7): e0130216.
- Mambanga P, Sirwali RN, Tshitangano T (2016) Factors contributing to men’s reluctance to seek HIV counselling and testing at Primary Health Care facilities in Vhembe District of South Africa. Afr J Prim Health Care Fam Med 8(2): e1-e7.
- Matovu JKB, Wanyenze RK, Wabwire-Mangen F, Nakubulwa R, Sekamwa R, et al. (2014) Men are always scared to test with their partners it is like taking them to the Police: Motivations for and barriers to couples’ HIV counselling and testing in Rakai, Uganda: A qualitative study. J Int AIDS Soc 17(1): 19160.
- Leta TH, Sandoy IF, Fylkesnes K (2012) Factors affecting voluntary HIV counselling and testing among men in Ethiopia: A cross-sectional survey. BMC Public Health 12(1): 438.
- Hlongwa M, Mashamba-Thompson T, Makhunga S, Hlongwana K (2020) Barriers to HIV testing uptake among men in sub-Saharan Africa: A scoping review. Afr J AIDS Res 19(1): 13-23.
- Mohlabane N, Tutshana B, Peltzer K, Mwisongo A (2016) Barriers and facilitators associated with HIV testing uptake in South African health facilities offering HIV Counselling and Testing. Health SA Gesondheid 21: 86-95.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Archive of Obstetrics Gynecology and Reproductive Medicine (ISSN:2640-2297)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)

